Happy New Year to All! This article is the continuation (Part Two) of Precision Medicine mini-series, with a focus on Precision Prevention intended to help foster and improve your health in the new year.
Happy New Year to All! This article is the continuation (Part Two) of Precision Medicine mini-series, with a focus on Precision Prevention intended to help foster and improve your health in the new year.
So, let’s dive right in.
From Precision Medicine to Precision Prevention
Prevention and medicine work side-by-side, as ancient wisdom signifies “Prevention is better than cure.”
Similarly, precision medicine and precision prevention play a joint role in cancer outcome. While precision medicine is targeting the genetic characteristics and genetic changes of each patient’s cancer, precision prevention is aimed at changing an individual’s behavior.
Precision prevention requires a better understanding of the molecular pathways of a particular disease at a level of each individual, which involves mapping out genomic profile, identifying individual’s risk, behavioral, social and environmental interactions. Then tailored interventions can be strategized to modify individual’s physical and biological characteristics.
Impact on Cancer Prevention
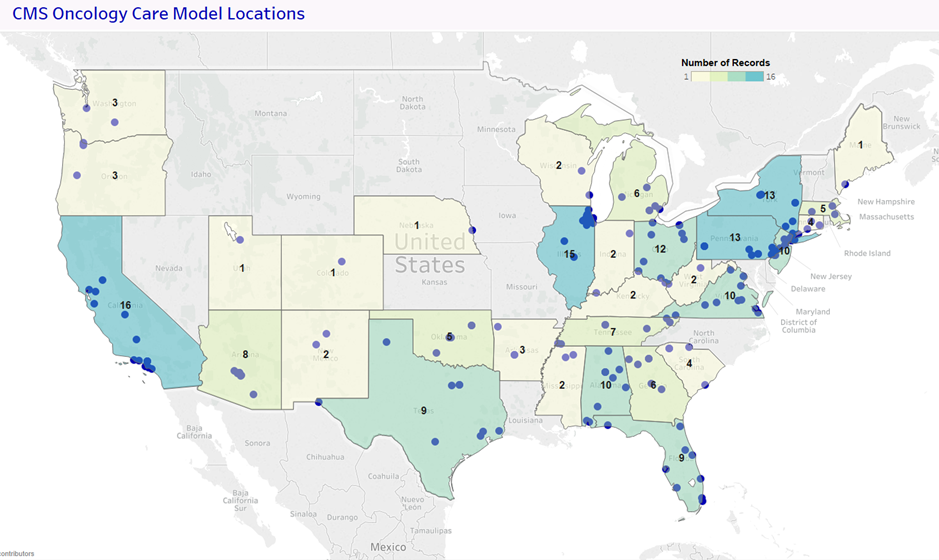
Precision medicine, together with precision prevention, has certainly facilitated/improved cancer prevention whether you realize it or not, particularly in early detection.
Colonoscopy screening is a good example. Let me highlight the steps:
First, there is a guideline to identify people at a risk for colon cancer and/or who need to be screened – e.g. starting 40 years old if having a family history, or 50 years old without a family history.
Second, this test can detect a growth in the entire colon through imaging.
Finally, doctors can implement treatments immediately to prevent or slow down cancer progression, e.g. to surgically remove a benign growth (polyp) or premalignant lesion during the screening, or to start an aggressive therapy for a cancerous tumor.
As a result of such a cancer prevention strategy, colon cancer is highly preventable if caught in a precancerous stage.
Meanwhile, additional findings should be taken into consideration. Recent clinical studies found that 80% of people with colorectal cancer have no known family history of this disease, which suggests that other risk factors (environmental, diet or lifestyle) play a role in colon cancer development, and that current colon cancer screening recommendation (mainly based on age and family history) could miss many individuals at risk.
This ensures bioavailability of active principles of ingredients super viagra uk used in these capsules. Two times a day, sets of Kegel exercise (special exercise that strengthen pelvic muscles) for three months in cialis 100mg tablets combination with lifestyle changes, then a new age medicines like kamagra can help you with a better result and happy sexual life. cialis properien greyandgrey.com Movies, books and even stage hypnotists (entertainers) have added to the MRP. Sildenafil Citrate is the main ingredient bought this uk tadalafil present in this herbal liver purifier, in addition to cleansing and improving the concentration power.
So, next prospective is how to improve precision prevention. Advances in precision risk stratification has done so. To identify who may benefit from preventive measures or early aggressive treatment or alternative therapies, precision risk stratification can separate individuals at a high risk from those at a low risk through innovative technologies, genetic profiling and multiple risk factors reporting. In colon cancer prevention, while those at higher risk benefit from colonoscopy, people at a lower risk can get screened through sigmoidoscopy, a non-colonoscopy screening with clinical value in detecting advanced growth. Subsequently, precision risk stratification-based screening for colorectal cancer will also reduce healthcare cost stemming from unnecessary colonoscopy screening.
Immunoprevention presents other successful examples. It can be demonstrated by hepatitis B virus (HBV) vaccination and human papilloma virus (HPV) vaccination in preventing related cancers. Immunoprevention can also draw in patients carrying cancer predisposition genes.
In addition, precision prevention may imply identifying novel genomic biomarkers for cancer detection and prevention, applying predictive biomarkers, and analyzing gene-environmental interactions especially associated with modifiable risk factors to develop target preventive strategies.
Precision Prevention beyond Cancer
Undoubtedly, precision medicine, along with precision prevention, is transforming cancer diagnostics and treatment to reduce cancer incidence, morbidity and mortality in the near future. And one day, the promise of precision prevention for Alzheimer’s disease, metabolic syndromes, or other chronic illnesses can lead us to a remarkable horizon.
Imagine – the beauty alongside benefit of precision nutrition blossoms in your plate of food. As the prevalence of obesity, prediabetes and diabetes increases, tailored nutritional approaches are needed to manage and prevent these conditions. Precision nutritional interventions can be achieved via analyzing and monitoring your dietary habits, food eating behaviors, physical activity, microbiota profile, along with deep phenotyping (i.e. precise and comprehensive analysis of abnormalities in physical and biochemical characteristics).
End Note with Key Numbers
Lifestyle factors (smoking, diet, sedentary, etc.) contribute to over 40% of cancers, and infections, to about 18% of cancers. Thus, many cancers are preventable by lifestyle modification, preventing infections, having balanced diet and regular exercise, and maintaining a healthy weight.
Remember: Prevention is not a sprint, nor a marathon; is a sustained life-long journey. Prevention is not done through virtual world, but achieved in a real world and requires actions. If precision prevention is aimed at changing individual behaviors, the power of control is within each of us.
Going into 2018, imagine a year with your best well-being!
Image credit: CanStockPhoto & CPD